Intralipid Treatment Vs. IVIg for Reproductive Failure



By Carolyn Coulam, M.D. and Nancy Hemenway
Failure to reproduce is a physically and emotionally challenging ordeal. When reproductive failure is repetitive feelings of shame, of grief and loss and failure are magnified. Before embarking on an effective and successful treatment plan patients need to determine the causes of their inability to conceive and to carry a pregnancy to termThere are many reproductive variables that can delay, interrupt or disrupt a pregnancy. Some of these include:
- Chromosomal Anomalies (i.e. Numerical chromosomal abnormalities or aneuploidies Extra Chromosomes or trisomy, Missing chromosome –monosomy)
- Anatomic Abnormalities (i.e. Missing or blocked fallopian tubes, Misshaped uterus)
- Hormonal Irregularities (i.e. Elevated FSH, Low Progesterone, Irregular levels of gonadotropin releasing hormone – GnRH)
- Immunological Issues (See article) and
- Thrombophilic Abnormalities (Blood clotting disorders)
Patients should not use their obstetrical history alone to determine whether an immunological reproductive issue exists. This means women may experience reproductive failure even after one or more successful full term pregnancies. When implantation failure occurs or when there is a loss after successful attempts, immunotherapy will be useful.
Be aware that only patients experiencing reproductive failure with an immunologic cause are expected to respond to immunotherapy. Patients who have unexplained infertility should consult a reproductive endocrinologist with reproductive immunological experience to determine if immunotherapy may be a consideration. Not all reproductive clinics have this physicians with reproductive immunological expertise or the correct lab assays to evaluate needs for immunotherapy.
The most frequently studied risk factors to identify an immunologic cause of reproductive failure have traditionally included the presence of antiphospholipid antibodies (APA) and elevated natural killer (NK) cells.
Elevated APAs are equally prevalent among women experiencing unexplained infertility, recurrent implantation failure, and recurrent pregnancy loss. It is important to note that Heparin and aspirin are successful in the treatment of elevated APA among women with a history of recurrent miscarriage but not with recurrent implantation failure. Intravenous immunoglobulin (IVIg) has been successful in the treatment of recurrent miscarriage and recurrent implantation failure among women with elevated APA and/or NK cell activity. Because of the very high cost (as much as $125,000 for treatment throughout pregnancy) and potential risks of IVIg, a blood product, alternative were pursued.
What is Intralipid?
Lipid is a descriptive term. The lipids are a group of fats and sterols. The term “Lipid” is descriptive rather than a chemical name such as “protein” or “carbohydrate.” Lipids include true fats (esters of fatty acids and glycerol); lipoids (phospholipids, cerebrosides, waxes); and sterols (cholesterol, ergosterol found in plants).
Intralipid is a brand name for an IV solution that has been made suitable to give IV to patients. The lipid has been broken into small droplets and suspended in water. Intralipid is a combination of liquid, lipid, and an emulsifying system suitable for intravenous.
Intralipid is the brand name for an IV medication used primarily to add calories to a patient. However, a number of studies suggest that Intralipid modifies or controls some immune functions including suppression of NK cells ability to destroy and become toxic to the cells.
These studies also suggest that Intralipid suppresses the pro-inflammatory cytokine generations of cells. Cytokines are any of more than 100 proteins produced by the white blood cells. Pro-inflammatory cytokines are the circulating substances in the blood that deplete lean body mass during a critical illness. They include several types of cytokines – interleukins (IL-1, IL-6, and IL-8) and also tumor necrosis factor (TNF) secreted by NK cells. TNF provides the body’s defense against disease and gives the killer cells killing power. We all have NK cells. Sometimes the TNF secretions destroy cells that are perceived to be foreign bodies, a virus or tumor when in fact they are destroying a fetus. (See Immunology may be key to pregnancy loss article.)
Recently, in an in vitro assay, Intralipid shows capacity to suppress NK cytotoxicity with equal effectiveness as IVIg
The first week after an Intralipid infusion, 78% of women experiencing reproductive failure who had elevated NK activity showed NK’s ability to destroy cells was suppressed to within normal range.
For the remaining 22%, the NK activity was also suppressed to within normal range after 2 or 3 infusions of Intralipid, given at 2-3 week intervals.
The duration of the suppression of the NK cell activity after normalization of NK cells with Intralipid infusions lasted between 4 and 9 weeks with the majority lasting 6-9 weeks during the first trimester of pregnancy.
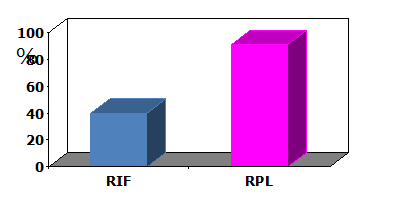
The pregnancy outcomes of 200 women experiencing recurrent reproductive failure who had elevated NK cell activity and who were treated with Intralipids are shown in Figure1
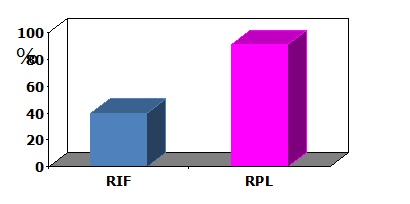
Figure 1. Successful pregnancy rates with Intralipid treatment
The pregnancy rate per cycle of treatment with Intralipid for women experiencing recurrent implantation failure with elevated NK cell activity was 52%. Among those women with a history of reproductive failure who became pregnant, the pregnancy loss rate was 9% and live birth or ongoing pregnancy rate was 91%.
When the pregnancy outcomes of women with a history of reproductive failure and elevated NK cell cytotoxicity treated with intralipid were compared with age- and indication-matched women treated with IVIg, no significant differences were seen as shown in figure 2.

Figure 2. Comparison of live birth rates among women with a history of reproductive failure and elevated NK cytotoxicity treated with IVIg and Intralipid.
The overall live birth pregnancy rate per cycle of treatment was 61% for women treated with Intralipid and 56% with IVIg.
While the mechanism by which intralipids suppresses NK function is not known, effects of fatty acids have been demonstrated to be mediated through receptors such as peroxisome proliferator-activated receptors (PPARs), G-protein-coupled receptors, and CD1 receptors as shown in figure 3.
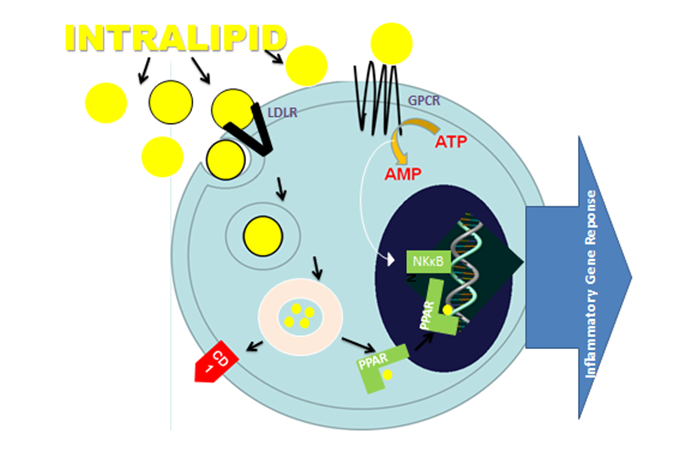
Figure 3. Pathways involved in fatty acid actions
Intralipid 20& is a sterile fat emulsion prepared for intravenous administration. It is made up of 20% soybean oil, 1.2% egg yolk phospholipids, 2.25% glycerin and76.5% water. The fatty acid components of the soybean oil include:
- Linoleic acid 44-62%
- Oleic acid 19-30%
- Palmitic 7-14&
- Linolenic 4-11%
- Stearic 1.4-5.5%
The major fatty acid component is linoleic acid. A number of studies have demonstrated conjugated linoleic acid improves reproduction in cows. Furthermore, conjugated linoleic acids have recently been shown to attenuate LPS-Induced proInflammatory gene expression by Inhibiting the NF-κB translocation through PPAR (see figure 3).
Summary
Intralipid is effective in the treatment of women experiencing reproductive failure who display elevated NK cell activity. A controversy that has occurred involves answering the general question ‘Does immunotherapy for treatment of reproductive failure enhance livebirths?’ The answer to the question is yes, BUT a treatment is more likely to work if it is given to those with physiological abnormality that the treatment can correct, and, if the treatment in fact corrects it. Elevated levels of NK cell cytotoxicity have been linked to recurrent miscarriage and recurrent implantation failure. Increased killing activity can be the result of elevated numbers of NK cells or increased cytotoxicity within each cell. Detection of elevation of circulating CD56+ (NK) cells and NK cell activity has been shown to be helpful in identifying individuals at risk for not implanting embryos and for losing karyotypically normal pregnancies . While both IVIg and intralipid are effective in suppressing NK cell cytotoxicity and enhancing live births among women experiencing reproductive failure who display elevated NK cell activity, only IVIg has been shown to enhance live births in women displaying APAs. The results of published studies suggest that intralipid can be used successfully as a therapeutic option to modulate abnormal NK activity in women with reproductive problems. Patients carrying chromosomally abnormal pregnancies and patients with anatomic or thrombophilic risk factors including APAs should not be treated with intralipid since they would not be expected to respond to intralipid therapy.
Carolyn Coulam MD will answer your questions here
